The 2024 Lung Cancer OncTalk was a live, virtual, interactive patient education event presented in December 2024, moderated by Dr. Ibiayi Dagogo-Jack...
VIDEOS
In this video series from ASCO 2024, Drs. Aakash Desai and Fauwzi Abu Rous discuss trial dates and clinical data as presented at the 2024 ASCO. To...
The panel discusses treatment options for a patient diagnosed with EGFR Exon 19 Deletion NSCLC and examines data from the Laura Trial, a patient with...
La Dra. Estelamari Rodríguez presenta información básica sobre el NSCLC EGFR+ y analiza la importancia de las pruebas de biomarcadores en el cáncer de...
¡El vídeo completo bajo demanda está disponible para verlo! Este evento educativo para pacientes, en directo, virtual e interactivo, incluye...
ARTICLES
Da click aquí para más información y para registrarte ahora Este 9 de agosto, no te puedes perder nuestro Foro anual de pacientes de terapias...
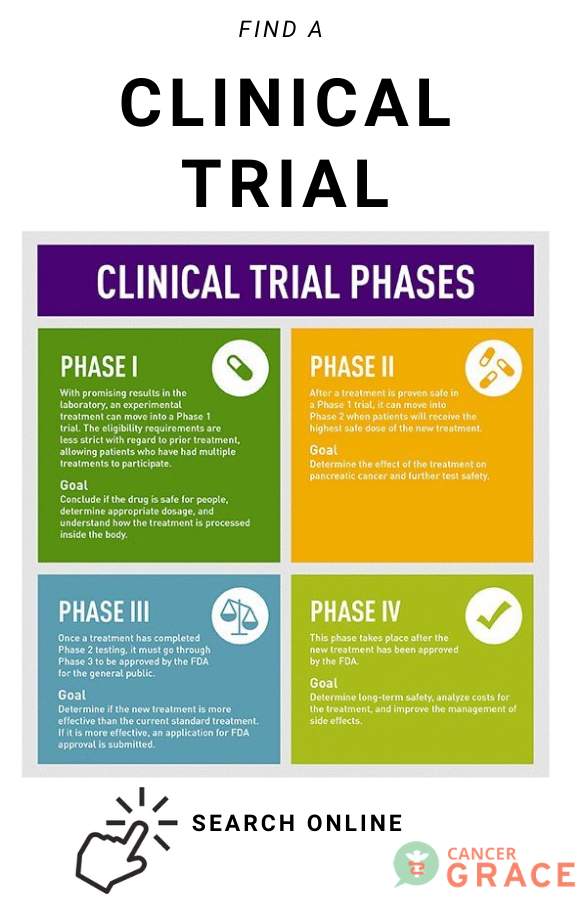
Tell your story and help us help others! Apply online now for this paid opportunity. This program gives a voice to those who have experience in participating in a clinical trial for a cancer diagnosis. Your voice helps to educate and advocate for others who are in or who may be considering a clinical trial. We want to hear from you!
Este 20 de julio no te puedes perder nuestro Foro anual de pacientes de terapias dirigidas de cáncer pulmón de GRACE en ESPAÑOL. Es un evento...
View the full Targeted Therapies in Lung Cancer Patient forum from 2023 in YouTube and embedded here!
Únete a nosotros, sábado 12 de agosto a las 9:00 a.m. En este foro anual de pacientes en vivo, los principales oncólogos torácicos de todo el mundo...
COMMUNITY FORUM
Hi All, I am a newbie so forgive me if I am posting in the wrong area of the forum. I recently had my first LDCT Lung Cancer Screening Scan and the...
I am a 15 year old male and have been vaping THC pens for about a year, sometimes I take breaks but do it pretty daily, About 3 days ago after vaping...
I’m a 33, turning 34 next month healthy female- In the past 4 months my dr has been watching my bloodwork for a slightly elevated d dimer .55 and ha...
First things first, my sincere thanks for maintaining this forum in which people with a diagnosis or a suspicion of lung cancer can raise our doubts...
My brother (Dhinesh) and I are caregivers to my mother Mrs. Hemavathi Bai, aged 74, and who has been living with ALK+ lung situation since early 2016...