Welcome!
Welcome to the new CancerGRACE.org! Explore our fresh look and improved features—take a quick tour to see what’s new.
Written by Joshua Bauml, MD
September 2017
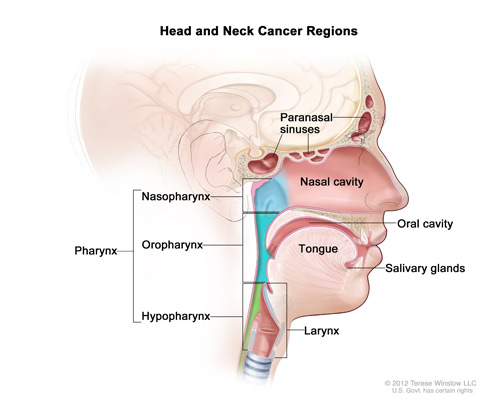
“Head and neck cancer” is an umbrella term for different cancers that occur in the head and neck region, from the sinuses and nasal cavity down to the larynx. The most common of these tumors affect the lining of the mouth and throat. Head and neck cancers are divided by where they start:
Oral cavity (tongue, gums, inner cheek)
Nasopharynx (where the back of your nose meets your throat)
Oropharynx (tonsils and base of the tongue)
Larynx (voice box); and
Hypopharynx (the region of your throat between the oropharynx and larynx).
Some of the most common presenting symptoms are a lump or swelling in the neck, a sore or spot in the mouth that does not heal, a lingering sore throat, pain or an inability to swallow, or a change in voice.
There are three major risk factors for head and neck cancer
Tobacco and alcohol use. Historically, this was the major risk factor. Tobacco and alcohol-related cancers can arise in any part of the throat. Men in their 60s and older are diagnosed more often with these cancers.
Epstein Barr Virus is one of the leading causes of cancer arising in the nasopharynx (where the back of your nose meets your throat). Epstein Barr-related cancer is rare in the United States, but is a major risk factor for patients in Asia. In the United States, most nasopharyngeal cancer is related to tobacco and alcohol use.
Human Papillomavirus (HPV) is an emerging cause of cancer of the oropharynx (base of tongue and tonsils). It is currently thought to be the primary cause of 60 – 80% of oropharyngeal cancers, depending on the population studied. Within the next few years, researchers expect HPV-related oropharyngeal cancer to become the most common HPV-related cancer, surpassing cervical cancer. This is likely because while there is a screening test for HPV infection in the cervix (Pap smears) there is no equivalent test for oropharyngeal cancers. HPV transmits through sexual contact. Patients who get HPV-associated oropharyngeal cancer tend to be younger (in their 40s or 50s) and have less history of tobacco use. Males are more likely to get HPV-associated oropharyngeal cancer. The prognosis of HPV-associated oropharyngeal cancer is much better than other types of head and neck cancers, but it remains a serious. See our webinar series about HPV-related head & neck cancer.
Who treats head and neck cancers?
Your team of medical professionals should include medical and radiation oncologists, plastic surgeons specializing in the head, neck, and dental regions, a dietician, and a speech pathologist.
What should I look for in a doctor to treat my head & neck cancer?
Try to find a care team with significant experience treating head and neck cancers – the anatomy of the head and neck is complicated, and a focused understanding of the disease will likely lead to better outcomes.
What is the standard treatment?
Your treatment will vary depending on the location of the primary cancer, its stage, and your age. Treatment may include surgery, radiation, chemotherapy, and targeted therapy. At this time, immunotherapy is only used in metastatic, or stage IV, head and neck cancer.
See:
Late Stage Oropharynx Cancer, Treatment and Side Effects
HPV-Related Head & Neck Cancer – current treatments and clinical trials
What are the side effects from treatment?
Side effects from head and neck cancer treatments depend on the treatment
Chemotherapy side effects may include hair loss, nausea and vomiting, lowered blood counts, hearing loss and ringing in the ears, neuropathy, and kidney damage
Erbitux (drug name: cetuximab), an antibody therapy frequently used in head and neck cancer, can cause an infusion reaction, rash, hair changes, and diarrhea
Radiation side effects may include taste changes, secretions, mouth or throat pain, skin discoloration
See also:
Late Stage Oropharynx Cancer, Treatment and Side Effects
Late Stage Oropharynx Cancer, Chemotherapy – Options and Practice
Will I be able to work while I receive treatment?
Every patient tolerates treatment differently. If you are receiving chemo-radiotherapy or radiation, you will likely have treatment five days per week for about seven weeks which can make it difficult to continue working full-time. Also, towards the end of treatment, side effects can accumulate, making work difficult. If you are receiving surgery, many patients can go back to work shortly after the surgical recovery. If you are receiving chemotherapy alone, it depends upon the regimen used. Talk to your doctor for more individualized advice.
Please feel free to offer comments and raise questions in our
discussion forums.
Dr. Singhi's reprise on appropriate treatment, "Right patient, right time, right team".
While Dr. Ryckman described radiation oncology as "the perfect blend of nerd skills and empathy".
I hope any...
My understanding of ADCs is very basic. I plan to study Dr. Rous’ discussion to broaden that understanding.

An antibody–drug conjugate (ADC) works a bit like a Trojan horse. It has three main components:
Bispecifics, or bispecific antibodies, are advanced immunotherapy drugs engineered to have two binding sites, allowing them to latch onto two different targets simultaneously, like a cancer cell and a T-cell, effectively...
The prefix “oligo–” means few. Oligometastatic (at diagnosis) Oligoprogression (during treatment)
There will be a discussion, “Studies in Oligometastatic NSCLC: Current Data and Definitions,” which will focus on what we...
Radiation therapy is primarily a localized treatment, meaning it precisely targets a specific tumor or area of the body, unlike systemic treatments (like chemotherapy) that affect the whole body.
The...

Welcome to the new CancerGRACE.org! Explore our fresh look and improved features—take a quick tour to see what’s new.
A Brief Tornado. I love the analogy Dr. Antonoff gave us to describe her presentation. I felt it earlier too and am looking forward to going back for deeper dive.